The gut microbiome, a heterogeneous community of trillions of microorganisms, is increasingly recognised as a key factor in various diseases, including disorders such as Metabolic Syndrome (MetS). The gut microbiome is thought to be involved in MetS, influenced by factors such as a compromised gut barrier, bile acid metabolism, antibiotic use, and microbially produced metabolites.
While research is ongoing, it is evident that the microbiome plays a significant role in various metabolic conditions. The challenge lies in determining whether changes in the microbiome are rather the cause or the effect of metabolic disorders, as factors like diet and lifestyle influence both. Understanding the complex relationship between the gut microbiome and metabolic disorders is crucial for developing effective prevention and treatment strategies.
Over Two Decades of Groundbreaking Research
Since Joshua Lederberg popularised the term ‘microbiome’ in 2001, over 15,000 academic articles have been published on the subject. The definition of microbiome is ‘the ecological community of all commensal, symbiotic, and pathogenic microorganisms that share our body space’ (1). It is now well established that the intestinal microbiota plays a role in maintaining health and contributing to the development of disease (2–6). Despite extensive research into the microbiome’s involvement in diseases, syndromes, and conditions, much remains to be discovered.

The intricate nature of the microbiome and the difficulty of accessing certain body sites have made it challenging to identify exact mechanisms and patterns in human research. Consequently, the approach to Metabolic Syndrome (MetS) in microbiome research has been to first decouple the risk factors and investigate separately whether there are microbial links to, for example, obesity, dyslipidaemia, and cardiovascular disease. This is because MetS is a combination of risk factors rather than a single condition (7–10).
Microbiome, Diet and Obesity: A Dynamic Relationship
The rising prevalence of obesity across both Western and non-Western countries is a major factor contributing to the growing medical focus on MetS (11). While obesity has traditionally been viewed as the result of an imbalance between energy intake and expenditure, emerging research shows that body weight regulation is far more complex (12). In the context of MetS, it is essential to consider an individual’s unique metabolic processing of food, as well as their genetics, lifestyle, and gut microbiome.
The gut microbiome, while responsive to fluctuations in caloric intake (13, 14), is particularly sensitive to the composition of one’s diet. This was effectively demonstrated in a study by David et al., where participants were placed on either a plant-based diet (grains, legumes, fruits, and vegetables) or an animal-based diet (meats, eggs, and cheeses) for five consecutive days. Results revealed notable changes in the microbiota over this short period. Participants on the animal-based diet saw an increase in bile-tolerant microbes such as Alistipes, Bilophila, and Bacteroides, along with a reduction in fibre-fermenting bacteria (14).
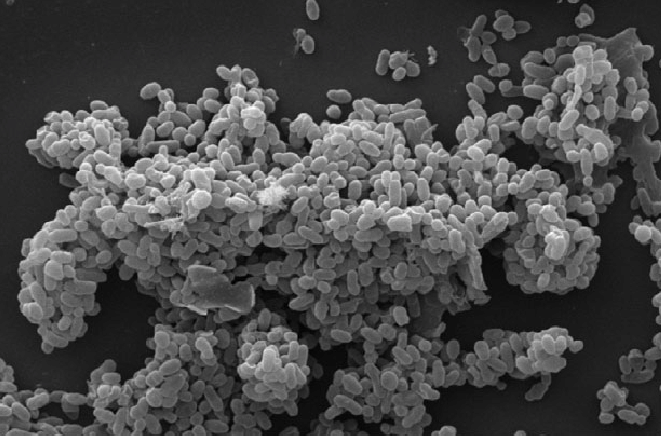
Further studies have reinforced the notion of microbiome sensitivity to various dietary factors, including the types of fat (15, 16), fibre (17, 18), and consumed food additives (19, 20). Animal studies have also shown the effect of diet on gut microbiome. In one study, Caesar et al. found that rats fed a lard-based diet experienced an increase in the pro-inflammatory bacterium Bilophila wadsworthia, whereas those fed a fish oil-based diet saw a rise in beneficial bacteria like Lactobacillus and Akkermansia muciniphila (21). Notably, higher levels of A. muciniphila have been linked to lower incidences of obesity, type 2 diabetes, and hypertension (22–24).
Other Factors Influencing Microbiota
While diet remains the primary factor influencing the gut microbiome, external environmental factors also play a role. Modern technological advances, such as artificial lighting and shift work, allow humans to manipulate their light-dark cycle. Alas, this can disrupt the natural 24-hour circadian rhythm on which the body’s biological processes, including hormone release and blood glucose regulation, are based (25–27). Such disruptions have been linked to obesity (28, 29), impaired insulin sensitivity (30), and lipid metabolism disturbances (31).
At the gut level, intestinal hormones and immune cells naturally fluctuate in a diurnal pattern under normal conditions (32, 33). Recent research has shown that disturbances to the gut microbiota, whether through antibiotic use or chronic consumption of a high-fat diet, can lead to circadian disruptions, which in turn promote weight gain and abnormal glucose regulation (34, 37). Taken together, we can see there is an evolving body of research that highlights the critical relationship between diet, life habits, gut microbiome, and the development of obesity, while also suggesting potential pathways for intervention.
Influence of Bacterial Byproducts on Blood Lipid Imbalance
Dyslipidaemia is defined as an abnormal concentration of lipids in the blood, with the diagnostic criteria identifying it as an elevation in triglycerides or a reduction in HDL (38). Dyslipidaemia and the resulting atherosclerotic plaques remain significant risk factors for cardiovascular disease and are often associated with impaired glucose metabolism and obesity. To uncover the underlying causes and potential solutions to dyslipidaemia, scientists have increasingly turned to the microbiome for insights.
Short-chain fatty acids (SCFAs) are the metabolic end products of microbial fermentation of dietary fibre from food and have the potential to play a role in mitigating the consequences of long-standing dyslipidaemia. While the human gut lacks the necessary enzymes to break down certain foods, particularly complex carbohydrates in the form of dietary fibre, specific anaerobic bacteria residing in the caecum and large intestine can ferment these fibres into a range of by-products.
The most notable of these by-products are acetate, propionate, and butyrate (39). The majority of acetate bypasses the circulation in the gastrointestinal organs to be oxidised, while the remaining acetate is converted to butyrate. Butyrate is a key substance that supports the intestinal epithelium, and its levels have been shown to be reduced in patients that have inflammatory diseases (40, 41).

It should be noted that microbial components may also increase health risks. While SCFAs can positively impact overall health, components such as lipopolysaccharide (LPS) and peptidoglycan -components of bacterial cell walls- are recognised by the host immune system and can contribute to an increased risk of cardiovascular disease (42).
Further compelling evidence suggests that the microbiome plays a role in the development of cardiovascular disease. Some studies indicate that the gut microbiome is integral to the conversion of dietary phosphatidylcholine into trimethylamine N-oxide (TMAO), a molecule linked to an increased risk of atherosclerosis (43, 44). Indeed, patients with atherosclerosis exhibited considerably elevated levels of circulating TMAO compared to healthy controls (44).
The evidence indicates that microbial metabolites, particularly SCFAs derived from dietary fibre fermentation, may offer protection against dyslipidaemia and MetS. Conversely, other bacterial metabolites -including TMAO, secondary bile acids, and bacterial cell wall components such as LPS- may act as drivers or significant contributors to these conditions.
The Gut Microbiome as a Dietary Biosensor?
The development of MetS results from a complex interplay between intrinsic host factors and extrinsic influences, such as dietary habits and lifestyle. While genetics is fixed, there is an opportunity to influence the gut microbiome to mitigate the risk of developing Metabolic Syndrome. Dietary factors are the primary cause of metabolic defects and have a significant impact on the gut microbiome, which is highly responsive to food quantity and composition, which could in that sense act as a dietary biosensor.
While research is ongoing, it is crucial to assess the impact of dietary choices on metabolism, taking into account the role of the gut microbiome. Despite the extensive body of research, the current gaps in knowledge regarding the microbiome’s role in metabolic diseases highlight the need for further investigation. Sustaining research efforts and maintaining a positive outlook are vital, as there is significant potential for further discoveries on the connection between the microbiome and metabolic conditions.
Bibliography:
- Lederberg J, McCray AT. ’Ome sweet ’omics — a genealogical treasury of words. Scientist. 2001;15(7):8.
- Sekirov I, Russell SL, Antunes LC, Finlay BB. Gut microbiota in health and disease. Physiol Rev. 2010;90(3):859-904.
- Kataoka K. The intestinal microbiota and its role in human health and disease. J Med Invest. 2016;63(1-2):27-37.
- Fan Y, Pedersen O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. 2021;19(1):55-71.
- Chen Y, Zhou J, Wang L. Role and Mechanism of Gut Microbiota in Human Disease. Front Cell Infect Microbiol. 2021;11:625913.
- El-Sayed A, Aleya L, Kamel M. Microbiota’s role in health and diseases. Environ Sci Pollut Res Int. 2021;28(28):36967-36983.
- Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365(9468):1415-1428.
- Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2(5-6):231-237.
- Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med. 2011;9:48.
- Samson SL, Garber AJ. Metabolic syndrome. Endocrinol Metab Clin North Am. 2014;43(1):1-23.
- Hill JO. Understanding and addressing the epidemic of obesity: an energy balance perspective. Endocr Rev. 2006;27(7):750–761.
- Beli E, et al. Restructuring of the gut microbiome by intermittent fasting prevents retinopathy prolongs survival in db/db mice. Diabetes. 2018;67(9):1867–1879.
- Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–1031.
- David LA, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–563.
- Devkota S, et al. Dietary-fat-induced taurocholic acid promotes pathobiont expansion and colitis in Il10–/– mice. Nature. 2012;487(7405):104–108.
- Wan Y, et al. Effects of dietary fat on gut microbiota and faecal metabolites, and their relationship with cardiometabolic risk factors: a 6-month randomised controlled-feeding trial. Gut. 2019;68(8):1417–1429.
- Sonnenburg ED, Smits SA, Tikhonov M, Higginbottom SK, Wingreen NS, Sonnenburg JL. Diet-induced extinctions in the gut microbiota compound over generations. Nature. 2016;529(7585):212–215.
- Desai MS, et al. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell. 2016;167(5):1339–1353.e21.
- Chassaing B, Van de Wiele T, De Bodt J, Marzorati M, Gewirtz AT. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut. 2017;66(8):1414–1427.
- Suez J, et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature. 2014;514(7521):181–186.
- Caesar R, Tremaroli V, Kovatcheva-Datchary P, Cani PD, Bäckhed F. Crosstalk between gut microbiota and dietary lipids aggravates WAT inflammation through TLR signaling. Cell Metab. 2015;22(4):658–668.
- Zhang X, et al. Human gut microbiota changes reveal the progression of glucose intolerance. PLoS One. 2013;8(8):e71108.
- Yassour M, et al. Sub-clinical detection of gut microbial biomarkers of obesity and type 2 diabetes. Genome Med. 2016;8(1):17.
- Li J, et al. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome. 2017;5(1):14.
- Wright KP, McHill AW, Birks BR, Griffin BR, Rusterholz T, Chinoy ED. Entrainment of the human circadian clock to the natural light-dark cycle. Curr Biol. 2013;23(16):1554–1558.
- Badia P, Myers B, Boecker M, Culpepper J, Harsh JR. Bright light effects on body temperature, alertness, EEG and behavior. Physiol Behav. 1991;50(3):583–588.
- Vandewalle G, Maquet P, Dijk DJ. Light as a modulator of cognitive brain function. Trends Cogn Sci (Regul Ed). 2009;13(10):429–438.
- Broussard JL, Van Cauter E. Disturbances of sleep and circadian rhythms: novel risk factors for obesity. Curr Opin Endocrinol Diabetes Obes. 2016;23(5):353–359.
- Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction: a randomized, crossover study. Ann Intern Med. 2012;157(8):549–557.
- Pamidi S, et al. Obstructive sleep apnea in young lean men: impact on insulin sensitivity and secretion. Diabetes Care. 2012;35(11):2384–2389.
- Broussard JL, et al. Sleep restriction increases free fatty acids in healthy men. Diabetologia. 2015;58(4):791–798.
- Mukherji A, Kobiita A, Ye T, Chambon P. Homeostasis in intestinal epithelium is orchestrated by the circadian clock and microbiota cues transduced by TLRs. Cell. 2013;153(4):812–827.
- Thaiss CA, et al. Microbiota diurnal rhythmicity programs host transcriptome oscillations. Cell. 2016;167(6):1495–1510.e12.
- Wang Y, Kuang Z, Yu X, Ruhn KA, Kubo M, Hooper LV. The intestinal microbiota regulates body composition through NFIL3 and the circadian clock. Science. 2017;357(6354):912–916.
- Thaiss CA, et al. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014;159(3):514–529.
- Zarrinpar A, Chaix A, Yooseph S, Panda S. Diet and feeding pattern affect the diurnal dynamics of the gut microbiome. Cell Metab. 2014;20(6):1006–1017.
- Leone V, et al. Effects of diurnal variation of gut microbes and high-fat feeding on host circadian clock function and metabolism. Cell Host Microbe. 2015;17(5):681–689.
- Jellinger PS, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Cardiovascular Disease – Executive Summary. Endocr Pract. 2017;23(4):479–497.
- Canfora EE, Jocken JW, Blaak EE. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol. 2015;11(10):577–591.
- Mathewson ND, et al. Gut microbiome-derived metabolites modulate intestinal epithelial cell damage and mitigate graft-versus-host disease. Nat Immunol. 2016;17(5):505–513.
- Dillon SM, et al. Low abundance of colonic butyrate-producing bacteria in HIV infection is associated with microbial translocation and immune activation. AIDS. 2017;31(4):511–521.
- Brown JM, Hazen SL. The gut microbial endocrine organ: bacterially derived signals driving cardiometabolic diseases. Annu Rev Med. 2015;66:343–359.
- Wang Z, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472(7341):57–63.
- Tang WH, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575–1584.
Media:
- Scanning electron image of Akkermansia Muciniphila modified from: Zhang, Ting & Li, Qianqian & Cheng, Lei & Buch, Heena & Zhang, Faming. (2019). Akkermansia muciniphila is a promising probiotic. Microbial Biotechnology. 12. 10.1111/1751-7915.13410. Creative Commons Attribution 4.0 International
